Best Modern Therapies for Crohn’s Disease in 2025 sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset.
In the realm of medical advancements, the landscape of Crohn’s Disease treatment is constantly evolving. As we look towards 2025, exciting developments in therapies are on the horizon, promising new hope for patients battling this chronic condition.
Overview of Crohn’s Disease
Crohn’s Disease is a chronic inflammatory disorder that can affect any part of the gastrointestinal tract, causing inflammation, ulcers, and other complications. This condition is a type of Inflammatory Bowel Disease (IBD) and can lead to severe pain, diarrhea, fatigue, weight loss, and malnutrition if left untreated.Crohn’s Disease was first described by Dr.
Burrill Crohn and his colleagues in 1932, hence the name. Since then, it has become increasingly prevalent worldwide, with approximately 3 million people affected in the United States alone.
Common Symptoms of Crohn’s Disease
- Abdominal pain and cramping
- Diarrhea
- Weight loss
- Fatigue
- Bloody stools
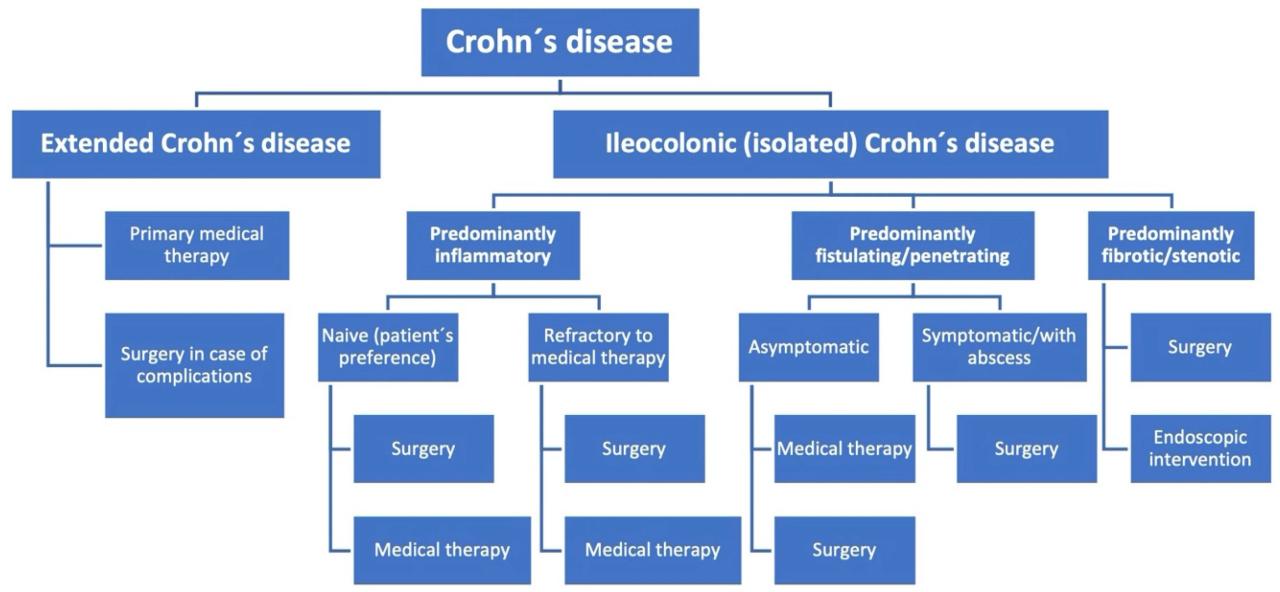
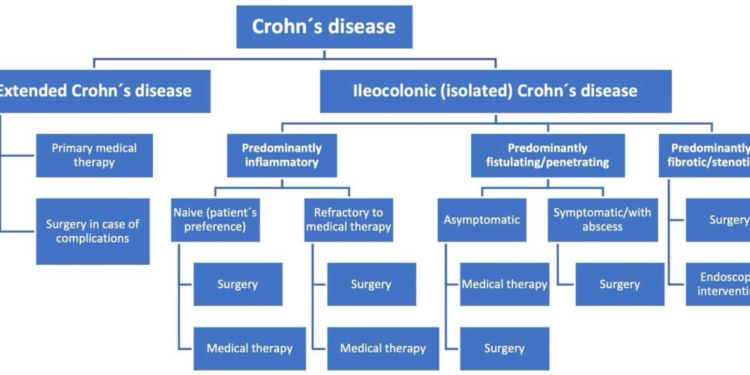
Current Treatment Landscape
Crohn’s Disease is currently managed through a variety of therapies that aim to reduce inflammation, control symptoms, and maintain remission. These treatments can be categorized into several main approaches, each with its own set of benefits and limitations.
Medication-Based Therapies
- Immunosuppressants: Drugs like azathioprine and methotrexate work by suppressing the immune system to reduce inflammation.
- Biologics: Targeted therapies like adalimumab and infliximab block specific proteins in the body responsible for inflammation.
- Steroids: Used for short-term symptom relief but not suitable for long-term use due to side effects.
Dietary and Lifestyle Changes
- Some patients find relief through specific diets like the low-FODMAP diet or the Specific Carbohydrate Diet.
- Regular exercise and stress management techniques can help improve overall well-being.
Surgery
- In cases where medications and lifestyle changes are ineffective, surgery may be necessary to remove damaged portions of the digestive tract.
- Surgery is not a cure for Crohn’s Disease and may come with its own set of risks and complications.
Limitations and Challenges
- Side Effects: Many medications used to treat Crohn’s Disease come with a range of side effects that can impact a patient’s quality of life.
- Effectiveness: Not all patients respond well to available therapies, leading to a trial-and-error approach to finding the right treatment.
- Cost: Biologic therapies can be expensive, making access difficult for some patients.
- Mental Health: Living with a chronic condition like Crohn’s Disease can take a toll on mental health, requiring additional support and resources.
Emerging Therapies in 2025
In 2025, there have been significant advancements in the treatment of Crohn’s Disease, with promising breakthrough therapies on the horizon. These modern therapies are paving the way for more effective and targeted approaches to managing this chronic condition.
Biologic Therapies
- One of the most exciting developments in Crohn’s Disease treatment is the emergence of new biologic therapies that target specific pathways in the immune system. These therapies work by reducing inflammation and helping to heal the intestinal lining.
- Unlike traditional treatments such as corticosteroids, which have broad immunosuppressive effects, biologic therapies are more targeted and can lead to better outcomes with fewer side effects.
Personalized Medicine
- Another promising approach in 2025 is the use of personalized medicine to tailor treatment plans to individual patients based on their genetic makeup, disease severity, and other factors. This precision medicine approach can lead to more effective outcomes and reduced risk of adverse reactions.
- By analyzing a patient’s genetic profile and other biomarkers, healthcare providers can identify the most appropriate treatment options, including biologic therapies, immunomodulators, or other medications.
Microbiome Modulation
- Researchers are also exploring the role of the gut microbiome in Crohn’s Disease and how modulating the composition of gut bacteria can influence disease activity. This emerging field of research holds promise for new therapeutic interventions.
- By targeting specific bacteria or using fecal microbiota transplantation (FMT), scientists aim to restore a healthy balance of gut microbes and reduce inflammation in patients with Crohn’s Disease.
Personalized Medicine Approach
Personalized medicine in treating Crohn’s Disease involves tailoring treatment plans to individual patients based on their unique genetic makeup, lifestyle factors, and disease characteristics. This approach allows for more precise and targeted therapies, ultimately leading to better outcomes for patients.
Benefits of Personalized Treatments
- Customized treatment plans: By considering individual genetic variations, personalized medicine can help create tailored treatment plans that are more effective and have fewer side effects.
- Improved patient outcomes: Personalized treatments can lead to better disease management, symptom control, and overall quality of life for patients with Crohn’s Disease.
- Optimized use of resources: By targeting therapies to specific patient profiles, personalized medicine can help avoid unnecessary treatments and reduce healthcare costs.
Role of Genetic Testing
Genetic testing plays a crucial role in tailoring therapies for individuals with Crohn’s Disease. By analyzing a patient’s genetic profile, healthcare providers can identify specific genetic markers associated with the disease and predict how they may respond to certain treatments.
This information allows for the selection of the most appropriate medications and dosages for each patient, maximizing treatment effectiveness while minimizing the risk of adverse reactions.
Technology and Digital Health Solutions
Technology has revolutionized the way Crohn’s Disease is managed, offering innovative solutions to improve patient care and treatment outcomes.
Use of Technology in Managing Crohn’s Disease
- Telemedicine platforms allow patients to consult with healthcare providers remotely, reducing the need for in-person visits and improving access to care.
- Mobile apps and wearable devices help patients track their symptoms, medication adherence, and diet, providing valuable data for healthcare providers to tailor treatment plans.
- Artificial intelligence and machine learning algorithms analyze vast amounts of patient data to predict disease flares and optimize treatment strategies.
Impact of Digital Health Solutions on Patient Care
- Digital health solutions enhance patient engagement and empowerment, allowing individuals to take an active role in managing their condition.
- Remote monitoring tools enable healthcare providers to monitor patients' progress continuously, leading to early intervention and personalized care.
- Virtual support groups and online resources offer emotional support and education to patients, improving their overall well-being.
Telemedicine and Remote Monitoring for Improved Treatment Outcomes
- Telemedicine consultations reduce barriers to care, particularly for patients in rural or underserved areas, ensuring timely access to specialists and expertise.
- Remote monitoring of vital signs, biomarkers, and disease activity allows for proactive management of Crohn’s Disease, preventing complications and hospitalizations.
- Integration of telemedicine and remote monitoring into standard care protocols has shown to enhance treatment adherence and quality of life for patients with Crohn’s Disease.
Lifestyle Modifications and Integrative Therapies
Living with Crohn’s Disease often requires more than just medical treatments. Lifestyle modifications and integrative therapies play a crucial role in managing symptoms and improving overall well-being.
Diet and Gut Health
Eating a well-balanced diet is key to managing Crohn’s Disease. Avoiding trigger foods such as dairy, spicy foods, and high-fiber foods can help reduce inflammation and discomfort. Opt for easily digestible foods like cooked vegetables, lean proteins, and whole grains.
Stay hydrated and consider keeping a food diary to track your symptoms.
Acupuncture and Yoga
Integrative therapies like acupuncture and yoga have shown promise in alleviating symptoms of Crohn’s Disease. Acupuncture can help reduce pain and inflammation, while yoga promotes relaxation and stress management. Consult with your healthcare provider to see if these therapies are suitable for you.
Conclusion
As we wrap up our exploration of the best modern therapies for Crohn’s Disease in 2025, it becomes evident that the future holds immense promise for improved patient outcomes and enhanced quality of life. With ongoing research and innovation, the journey towards better management of this complex disease continues, offering a beacon of hope for those affected.
Query Resolution
What are the key symptoms of Crohn’s Disease?
Common symptoms include abdominal pain, diarrhea, weight loss, fatigue, and malnutrition.
How do modern therapies differ from traditional treatments?
Modern therapies focus on precision medicine and targeted approaches, whereas traditional treatments are more generalized.
Can lifestyle modifications alone manage Crohn’s Disease?
Lifestyle changes can complement medical treatments, but a holistic approach involving both is usually recommended for optimal management.






![Natural Remedies to Treat Crohn's and Colitis [Slideshow]](https://medic.infogarut.id/wp-content/uploads/2025/12/Best-Treatment-for-Crohns-Disease-Expert-Insights-120x86.jpg)